I am currently dealing with my sixth health insurance company in four years and my eleventh since 2007 when I moved to Scottsbluff, Nebraska. None of these changes were of my doing. My employers decided to change companies. Each change was touted as something better for the employee, but, looking under the hood, as usual, it benefits the company more than the individual.
In the United States, if your employer offers health insurance which meets the 9.61% affordability requirement, then you are not eligible for subsidies under the Affordable Care Act (ACA). I have looked each year and I am not eligible for subsidies, but I can choose to get an ACA plan and pay thousands more for similar plans from my employer. If I were to switch to Paul’s insurance, the monthly cost would triple, totaling more than my net salary. So, I have to stick with what is offered through my employer.
In 2022, my coverage provided a three-month supply of my medications, with the exception of one, which has never made sense why. My doctor did not understand either, but I am limited to 12 pills every 15 days. We gave up fighting as it is an “as needed” pill and I instead play the stockpiling game for the times when I do need to take it every day.
One of my main medications is Lantus, a long-lasting insulin. I will be taking Lantus the rest of my life. My doctor prescribes a three-month supply every time it’s up for renewal. I honestly have never known if I was going to get a three-month or one-month supply when I went in for a refill. For all of 2021 and 2022, my insurance did not cover Lantus, so I had to get a coupon from the manufacturer, Sanofi, which brought the price down from $386 per month to $35 per month for two pre-filled pens.
I never knew when I went in if I was going to be paying $35 or $105, so I always made sure I had the $105 with me when I went to the pharmacy. In August 2022, I was given a three-month supply, but the cost was $140. No one could tell me why, including my insurance company. I only have suspicions, but this was around the time insulin was capped for those on Medicare and Medicaid. It makes sense the companies were shifting those forced cost cuts from the government onto regular folks like me. We can complain all we want about it, but there’s little we can do.
I tried not to be too pissed about it, but it was frustrating that the price was raised out of the blue and no one could answer why other than to say it was the insurance company’s decision. Yeah, okay. Whatever.
When I went in to renew my prescription in October for another three-month supply, I was given a one-month supply. It cost $35. Did you just go, “Wait. What?” Yeah, I did, too.
The pharmacy tried to increase it to a three-month supply, but was denied. I was only allowed one-month supplies from now on. The insurance company wouldn’t budge.
As 2023 began, my employer had shifted to another insurance company. It was touted as a great thing because our deductible was shifting from $4,000 to $2,000 and out-of-pocket from $6,000 to $4,000. Our monthly amount taken out of our paychecks remained unchanged. I would now have to pay $2,000 before the insurance company would cover anything.
Once the deductible is met, the company pays a portion of the $4,000 out-of-pocket and I pay a portion. This part of American health insurance is a nightmare because I never know what I have to pay. For one medication, I sometimes pay $4.22 and sometimes $0. Finally, once out-of-pocket is met, the company pays for everything else.
A couple of years ago, I met the deductible in March, only for my employer to change insurance companies. I was assured, I wouldn’t have to pay the deductible again, but I did. I ended up paying the monthly cost of insurance, plus $8,000 in deductibles before anything was covered. I paid until the first week in July, dipping into my savings account to purchase medication I need to live.
This year, between therapy, my yearly mammogram, and one medication, I had met the $2,000 deductible in January. Here’s the kicker though. I still had to keep paying because my insurance company insists on paper claim forms. Yeah, it’s 2023 and all medical claims must be mailed to their processing place in Pennsylvania. My therapist has been kind an not billed me yet this year as she is waiting for all the bullshit to be settled and doesn’t think it’s fair it takes months to process claims.
As I write this on May 1, the folks at the mammogram place, my doctor, and my therapist have yet to be paid. My deductible was officially met in early March solely through the cost of my prescriptions. This was when my insurance company started questioning my medications. I take a weekly medication I need to live. It costs $1,080 per month, but I have a coupon from the manufacturer which brings the price down to $783.46.
I take this medication on Wednesday mornings. I called in my refill on Thursday. The automated system said it would be ready Saturday. Between Paul and I, we went to the pharmacy on Sunday, Tuesday, and Wednesday. They told us it was in but not yet ready and they were waiting for something from my doctor. As Paul went the second time, he wasn’t sure what that meant. I didn’t either because I had five refills still on the current prescription.
When I went in on Wednesday, they said the insurance wanted justification and pre-authorization from my doctor as to why it was prescribed. My doctor said she never got a message from the pharmacy and was pissed. She called over to the billing department and they didn’t receive anything either. My doctor made an angry call to the pharmacy and then forwarded the request to billing with a “rush” notification. I finally got my prescription Friday evening. I fully expect this bullshit to repeat itself next year when everything resets and I get to do this stress-inducing dance again.
So, back to my Lantus. Once my insurance company started being forced to pay for my prescription, they started in with their shenanigans. Remember, I was paying $35 a month for two pens, which is a month’s supply.
With my deductible met, I can only get one pen. The insurance company had an absolute shit reason for this limit.
“Why can I only get one pen?” I said.
“Because that is a month’s supply,” the insurance representative said.
“No, two pens are a month’s supply,” I said.
“Two pens are a 32-day supply,” the insurance representative said. “We only cover a 30-day supply, which is one pen.”
“Wait. What? That’s stupid,” I said. “There are plenty of months with 31 days.” I really wanted to say more and something else, but bit my tongue.
“One pen is a 30-day supply for you and we only cover a 30-day supply,” the insurance representative said.
“But one pen is only good for 16 days,” I said.
“We will only cover a 30-day supply,” The insurance representative said. “Two pens are a 32-day supply.”
I tried to reason with the representative, explaining the two extra days, and thus two pens, would be cheaper. Nope. No dice. I tried get a three-month supply, but they will only cover a 30-day supply.
So, now, instead of paying $35 for a month’s supply of insulin, I pay $35 every 15 days. I get to pay double for my medication because some fuckhead bean counter somewhere decided this will somehow save the company money. I wonder if I will magically be shifted back to three-month supplies once my out-of-pocket is reached and the company has to pay the full amount. I haven’t done the math on that to know if it really is cheaper and I’m tired of fighting every 15-20 days with the pharmacy and the insurance company.
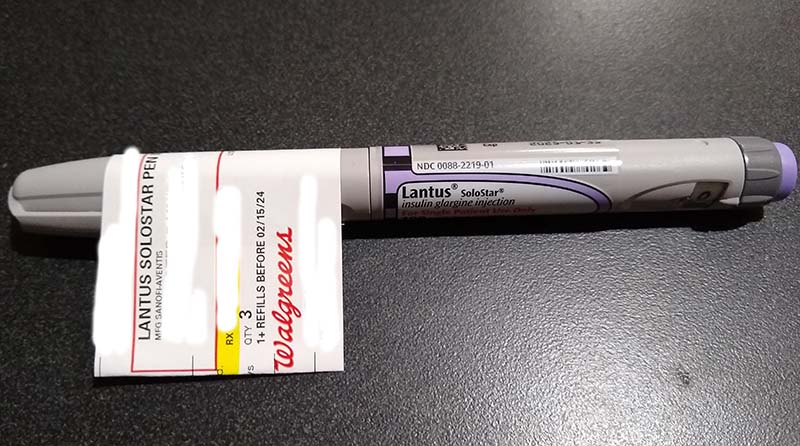
The photo at the top of my post is how I received my Lantus pen in April. The prescription label was stuck partially onto the pen and placed in a paper bag. At least when I got two or more pens, the pens were placed in a Ziploc baggie before being placed in the paper bag and the label was on the baggie. Somehow, this meets requirements of safe handling of medications and I have to trust that no one has tampered with my insulin pen.
I’m not begrudging folks on Medicare and Medicaid. They are finally getting cheaper insulin. I shouldn’t be surprised that the pharmaceutical companies are probably shifting costs onto regular working stiffs like me. American health care is a shit show and absolute garbage policies are screwing over regular citizens.
Paul and I plan to meet later this year with a coworker’s father who does health insurance for a living to find out which plan would be better for me in the future. The undue stress in dealing with trying to get my medication several days each month is too much for me. Paul has been great in offering to pick up my prescriptions, but he is growing increasingly angry at the uncertainty of it all and never knowing if he’s going to come home with my medication or not, as well as how it’s been affecting my mental health.
Oh, that coupon that I had from Sanofi? Yeah, I can’t use it anymore. So, even though the company’s website said I could and I printed the coupon and took it into the pharmacy, I can’t use it because of my insurance. No, I don’t understand why. No one does.
Money talks in this country and I have to spend mine on medication so I can live instead of lining politicians pockets.

Leave a Reply